What is PRRT?
PRRT stands for Peptide Receptor Radionuclide Therapy. Peptide refers to a small molecule that is very similar to the naturally occurring hormone somatostatin. We call it a somatostatin analog, meaning that it is similar but not identical to somatostatin. There are a number of somatostatin analogs that are use in patients with neuroendocrine tumors including octreotide, sandostatin, lanreotide. These peptides bind to the somatostatin receptor that is expressed on the majority of neuroendocrine tumor cells.
When binding to these receptors the peptide is brought into the tumor cell and stays there. Because neuroendocrine tumor cells are one of the few cells in the body that express somatostatin receptors, we are able to target our peptide to the tumor cells using the receptor. Radionuclide refers to the radiation that we attach to the peptide.
There are different types of radiation that we can use, but in PRRT all the radiation given off is the type that can be used to kill cells. Therapy refers to the idea that we are using peptides to target the receptors and bring the radionuclide into the tumor cells in order to treat the cells. That is PRRT.
What is PRRT? PRRT stands for Peptide Receptor Radionuclide Therapy, an FDA-approved therapy used for systemic treatment of neuroendocrine tumors.
Peptide refers to the small molecule for this therapy. The Peptide used (DOTATATE) is very similar to Somatostatin, a hormone which binds to receptors found on neuroendocrine tumors.
Receptor refers to a specific target on neuroendocrine tumor cells that the peptide attaches to. After the peptide joins with a Receptor, it becomes attached and enters the targeted tumor cell.
Radionuclide refers to radioactive atom that is attached to the peptide. As the peptide enters the cell, it brings the Radionuclide into the tumor cell. The radionuclide (lutetium-177), then decays and emits radiation within the tumor cell.
Therapy refers to the idea that we are using this combination of Peptides, Receptors, and Radionuclides to Treat these targeted tumor cells, improve symptoms, and extend life.
UCSF Helen Diller Family Comprehensive Cancer Center
Gastrointestinal Oncology
1825 Fourth Street, 4th Floor
San Francisco, California 94158
Appointments/Main: 415-476-2212
Fax: 415-353-9931
Commons Questions
- Do I qualify for PRRT?
There are many factors involved in deciding who will benefit from PRRT. If you have a Somatostatin-positive (+) Neuroendocrine Tumor, your Oncologist will review recommendation for treatment. A referral can be sent to our GI Oncology team, which should include recent biopsy results, imaging, visit notes, and any prior chemotherapy. If our team recommends that you receive PRRT, our PRRT Nurse Navigator will contact you to develop a specialized plan, and provide additional education.
- What if I live far away from UCSF?
UCSF is one of the few Destination Programs offering this FDA-approved therapy. Due to this, many patients travel from a long distance. Your dedicated PRRT Team will assist with coordinating blood tests and imaging close to your home, and a combination of video visits and in-person visits. Additional travel or financial resources can be reviewed with our Social Workers.
- What is a typical PRRT treatment schedule?
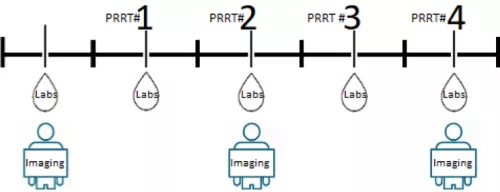
Our PRRT Nurse Navigator will assist you with scheduling of all appointments associated with PRRT. Treatment is typically administered in four in-person PRRT cycles. Each cycle is eight weeks apart. Between each treatment, your team will recommend blood tests and repeated imaging, tailored to your health and specific plan. Below is a common timeline for PRRT #1- PRRT#4.
- Will I stay in the hospital overnight?
PRRT is given as an outpatient appointment, which typically lasts four to six hours. Appointments take place in the UCSF Precision Cancer Medicine Building. Our Radiology Department will have a designated nurse, room, and restroom reserved for you. Once your infusions are complete, your team will clear you for discharge.
- What happens during each PRRT treatment?
Please check in with our Radiology Department 30 minutes prior to your appointment time. A team member will escort you to your designated treatment room, where your vital signs will be taken, and the nurse will start an IV in your arm. A Nuclear Medicine MD, our Radiation Safety Officer, and your PRRT Nurse Navigator will answer any remaining questions. You will receive Saline and an Amino Acid Solution through your vein for several hours. The PRRT dose only takes 30 minutes to infuse through your vein, and is not painful. Your clinical team will ensure your comfort throughout your appointment.
- Who will look at my test results during PRRT?
Neuroendocrine tumors require a team approach with many providers who work together. This approach is referred to as Multidisciplinary Care. This can include a Medical Oncologist, Surgical Oncologist, Nuclear Medicine Physician, Interventional Radiologist, and a Primary Care Doctor. If you are traveling from a distance, we will also be communicating with your local providers. Your PRRT Team will be reviewing any tests completed during your treatment schedule.
- What are possible side effects after PRRT treatment?
Every patient is different and may experience side effects differently. Common side effects include generalized fatigue, weakness, nausea, mild increase in flushing, mild increase in diarrhea, and changes in your bloodwork results. Although rare, Carcinoid Crisis can be the most severe side effect of PRRT and would occur within 24-48 hours of therapy. These symptoms could include severe flushing, sweating, palpitations, diarrhea, vomiting, severe abdominal cramping chest pain, or difficulty breathing. If these symptoms are present, call 911 and report to the nearest Emergency Room.
- What if I take a Long-Acting or Short- Acting Somatostatin Analog injections?
These injections can continue throughout PRRT, however we do have recommended timeframes for when each type of injection should or should not be given. Our Nurse Navigator will assist with coordinating your schedules, coordinating with your Medical Oncologist, and confirming that appointments can be adjusted accordingly.